Physio Blogfrom the team at South Coast Physiotherapy
Sunday, 31 August 2025 06:25
Understanding the Vestibular System and how Physiotherapy can help with Vertigo
The vestibular system helps us control balance, eye movements, and our sense of position in space. The peripheral vestibular apparatus is located in the inner ear and consists of the bony labyrinth—made up of three semicircular canals, the utricle, and the saccule. Conditions affecting this part of the system are referred to as peripheral vestibular disorders. When the vestibular system is disrupted, people may experience vertigo—commonly described by patients as dizziness, spinning, swaying, or disequilibrium. Common Peripheral Vestibular Conditions There are many medical causes of dizziness, so it is important that a medical evaluation by a GP, neurologist, or ENT specialist is undertaken. Some of the most common vestibular-related conditions include: Benign Paroxysmal Positional Vertigo (BPPV) Caused by dislodged calcium carbonate crystals (otoconia) moving into the semicircular canals. This leads to brief episodes of vertigo triggered by changes in head position such as rolling in bed or looking up. Menière’s Disease Thought to result from an abnormal build-up of endolymphatic fluid in the inner ear, causing episodes of vertigo, fluctuating hearing loss, tinnitus, and a sensation of fullness in the ear. Labyrinthitis Inflammation of the entire inner ear (labyrinth), usually viral, affecting both balance and hearing. It typically presents with acute vertigo, nausea, and hearing loss. Vestibular Neuritis Inflammation of the vestibular nerve, usually viral, impairing balance but not hearing. It is characterised by sudden onset of severe vertigo, nausea, and unsteadiness that may last for days. Physiotherapy and Vestibular Care Physiotherapists who have completed additional vestibular training play a vital role in the assessment and management of peripheral vestibular conditions. The most common cause of vertigo seen in physiotherapy practice is BPPV. BPPV and the Modified Epley Manoeuvre BPPV is typically diagnosed with a positional test (e.g. Dix-Hallpike), in which vertigo is reproduced and nystagmus (involuntary, repetitive eye movement)…
Friday, 19 July 2024 03:20
Achilles Tendinopathy
The Achilles tendon is one of the most commonly injured tendons in the body and unsurprisingly it is therefore an injury we see a lot of. This blog will be a quick run down on the fundamentals of what an Achilles tendinopathy is and how we treat them. What is a tendinopathy? Unlike an acute muscle tear or a broken bone a tendinopathy is a more complex multifaceted injury. It is generally an overuse injury where the tendon (tendons are what attach our muscles to our bones) has been repeatedly pushed beyond its capacity. These injuries are characterized by pain, a decline in function and reduced exercise tolerance. Structurally we see a disruption of the collagen fibres and a deregulation of the extracellular matrix – the building blocks of the tendon and why we see the reduced function. There is also increased inflammatory mediators and sensory nerve innervation – which explains the pain. Achilles Tendon We have tendons all over our body and these injuries are seen in the shoulder with rotator cuff tendons, the knee with the patella tendon and the hip with the gluteal tendons (as well as the elbow, wrist and groin). The Achilles tendon (named after the famous Greek Warrior God) is the largest and strongest tendon in the human body. It is approximately 15cm in length and rotates clockwise up to 90 degrees, running from the soleus and gastrocnemius muscles and inserting into the back of the heel. The tendon is surrounded by a paratenon allowing it to glide back and forth. It is made up of Type I collagen giving it the ability store and release energy so that it can stretch and recoil like a spring in response to the stretch/shortening cycle of the calf complex – an important action for locomotion. This…
Sunday, 17 December 2023 10:20
Calf Injuries
From Sam Kerr to Nathan Lyon to Will Skelton - calf injuries plagued our Australian sports stars through 2023. Injuries to this muscle complex are in fact a very common sporting injury with only hamstrings and quadriceps being more frequently injured in sporting populations. The superficial calf complex is known as the triceps surae and comprises of 3 muscles – the gastrocnemius, soleus and plantaris. Interestingly it has been found that injuries to the individual tricep surae muscles can be sport specific with American Football players mostly injuring the gastrocnemius and Australian Rules Footballers mostly injuring the soleus (1,2) A gastrocnemius strain will occur with a sudden ballistic movement with the knee in full extension. This is because the muscle attaches above the knee joint and is therefore exposed when the knee is fully extended. The injury is more prone in the medial head of the muscle – due to this part of the muscle experiencing more loads. A soleus strain is often associated as an overuse injury. This muscle attaches below the knee and is therefore loaded with the knee in flexion – although it is also loaded with knee extension. On examination these tears can have a palpable defect at the site of the tear if they are high grade. They will have pain when stretching the calf and on resisted plantar flexion movements such as performing a heel raise. These tears are categorized based on the degree of structural damage. Recently, with MRIs being more readily available, this process has become more specific which has allowed medical teams a more precise prediction of outcomes. One example of this is the British Athletic Classification, which is used globally, and groups muscle injuries based on the location of injury and the involvement of different soft tissue structures – along…
Thursday, 16 February 2023 10:16
Achilles Tendon Rupture - The importance of rehabilitation
Named after the famous Greek Warrior God the Achilles tendon is the largest and strongest tendon in the human body. It is approximately 15cm in length and rotates clockwise up to 90 degrees, running from the soleus and gastrocnemius muscles and inserting into the back of the heel. The tendon is surrounded by a paratenon allowing it to glide back and forth. It is made up of Type I collagen giving it the ability store and release energy so that it can stretch and recoil like a spring in response to the stretch/shortening cycle of the gastrocnemius and soleus muscles – an important action for locomotion. This unique structure allows the Achilles to withstand fast and dynamic loads, which can be up to 7 x a persons body weight during running and jumping activities (1). It also makes rehabilitation of this tendon very challenging. It is the most commonly injured tendon in the human body and complete ruptures are reported from 11 to 37 per 100,000 population and are currently on the increase (1). A ruptured tendon is when there is a complete full thickness tear through the tendon fibres. An Achilles rupture will often be a traumatic injury with acute pain and a sudden inability to walk. Patients describe a popping sensation at their heel and a feeling of being kicked. For the Achilles this injury has a bimodal age distribution with it occurring in 2 groups of the population – those between 25-40yrs and those over 60 yrs (2). It is generally an acute injury in the younger group and can be more of a chronic presentation in the older population – although as our aging population strive to remain active we are seeing an increasing number of acute ruptures in this older demographic. This bimodal age distribution…
Tuesday, 17 November 2020 10:31
Return to Exercise Post COVID
In the 15 years that I have been working as a physiotherapist I have never had a year quite like this one. Both at work and at home the COVID 19 Pandemic completely changed our daily routines from using Telehealth to treat patients to home schooling the kids (and in some cases doing both at the same time!!). Luckily here in Victoria we seem to be coming out of our second wave but, as we slowly move away from isolation and return to the golf course and the gym, we are seeing an increase in injuries related to these activities. The combination of lockdown restrictions disrupting our regular exercise and the loss of incidental activity with working from home (or from not working at all) have led to a more sedentary lifestyle for a large number of the population. We know that inactivity will lead to both muscle loss and reduced cardiovascular output which will directly affect your performance be it at the gym, on the golf course or in the garden. This deconditioning can be reversed with a gradual reintroduction of activity and often it does not need to be any more complicated than just returning to your activity at a lower intensity. However, if you do return straight to your previous level of activity then you will increase your risk of injury with the more senior population being most at risk of injury if attempting a direct return. To try and get an indication of how much condition you may have lost during the lockdown period simple body weight exercises specific to your activity can give you a good picture of where you are. For example, if you are looking at getting back to running but you are unable to perform a single leg heel raise then starting…
Saturday, 20 June 2020 22:32
Knee Osteoarthritis Program
Knee osteoarthritis is one of the most common joint diseases and is an expensive burden to health care across the globe. As a result there has been a push over the last 2 years to look at how non surgical management strategies can be improved. As I discussed in my blog ‘Happy Knees’ (click here to read) an area where non surgical management has failed in the past is by addressing knee OA as a purely mechanical and structural entity and not addressing the complexities of osteoarthritis and the associated biopsychosocial factors. Programs such as the GLA:D program in Europe and here in Melbourne have shown that incorporating education and general physical activity along side a physiotherapy monitored strengthening program have shown improvements in physical function as well as a reduction in pain medication and sick leave. (1) At South Coast Physiotherapy we are now able to offer our own knee program specifically for OA knees in line with these findings. It is a 12 week program and is designed to be specific to each individual, incorporating education, strengthening and physical activity. Having the program supervised by a physiotherapist ensures that the intensity and dosage of both strength exercises and physical activity is correct. The goals of this program are to promote self empowerment to each patient. By the end of the 12 weeks patients will have the knowledge, skills and confidence necessary to manage their knee symptoms and pursue an active life. We will explore how their knee pain is a modifiable symptom driven by sensitized structures rather than damaged structures and is influenced by a variety of biopsychosocial factors. It is not just people who are already experiencing OA related symptoms that would benefit from this program. Research shows a six fold increase in the likelihood of knee…
Tuesday, 05 November 2019 22:51
Happy Knees
The importance of addressing Knee Health in treating knee OA Osteoarthritis (OA) is a degenerative process involving the break down of cartilage at a joint leading to pain, swelling and loss of function. The prevalence of knee OA has doubled in the last 50 years and is a major burden on health care services around the world. As a result researchers and health organisations are constantly looking at the best ways to manage this condition. Clinical practice currently suggests that treatments should be directed away from structural/mechanical models which are based on restoring the knee structure and instead should be directed more towards addressing the health of the knee. Understanding that OA is more than just tissue breakdown and that if treatments can control the inflammatory process and tissue sensitivity associated with OA, that there will be an improvement in knee function, pain levels and patient quality of life. Cartilage is not related to pain Historically treatments have been structurally and mechanically based, directed towards restoring the lost cartilage either through different types of injections or supplements. However we know that the breakdown of cartilage is not correlated to knee pain and therefore focusing treatment on restoring cartilage will not necessarily make the knee feel or function any better. So why doesn’t my exercise routine work? Since I qualified as a physiotherapist back in the early 2000s exercise has been one of the first line treatments for the condition with focus on restoring range of motion and improving muscle strength. Studies have shown that it can effectively reduce pain and improve function and when you add this to the extensive list of health benefits that are associated with exercise it is not surprising that it is the first port of call. However even with exercise we need to ensure that…
Thursday, 04 July 2019 19:25
Reduce Injury Risk on the Slopes
When heading to the snow as a first timer or returning to the mountain for the first trip of the season it is important to prepare yourself for the snow conditions. Strategies and steps such as massage can be put in place to reduce the risk of injuries and other factors enabling you to get as much out of your snow trip as possible. When snowboarding and skiing we are utilizing muscles groups that we wouldn’t use on day to day bases therefore there is increased risk of injuries occurring. The main muscles groups used are core, hamstrings, glutes, quads, calves and as for beginners our arms from pushing yourself up. The common types of injuries that can occur for skiers and snowboarders are wrist fractures, ACL and knee injuries, whiplash, concussions, shoulder and elbow dislocations and dehydration. There are several benefits of massage pre and post your snow trip experience not only reducing the risk of injuries but also other aspects such as: - Increasing the removal of bio products, lactic acid and reducing muscle soreness (DOMS) - Increasing the recovery rate and reducing the rate of muscle fatigue therefore allowing more time on the hill - Massage increases Rom and flexibility which then improves proprioception and body awareness We can also look at others strategies such as strengthening exercises specific to muscle groups and for the individual, snow/safety gear as well as warm up and recovery programs heading on and coming off the mountain to ensure you get the best snow experience possible.
Tuesday, 21 May 2019 08:28
Coastrek 2019
We are excited to be providing physiotherapy cover for Coastrek 2019. This is a great annual event where participants trek across some of best coastal areas the Peninsula has to offer while raising thousands of dollars for the Fred Hollows Foundation To all you Trekkers about to take part in this grueling but equally rewarding event we have listed some tips on managing, and hopefully avoiding, common trekking injuries. Blisters Blisters are always a common complaint for any long distance walk and the key management protocol is to minimize friction and moisture. We would recommend to take a few spare sets of socks and change them regularly, particularly if you have stepped in a puddle or the incoming tide. We will be providing physiotherapy stations along the course and will be able to do blister taping where necessary. Pacing The best way to reduce risk of soft tissue injuries is completing a full training schedule specific to the tasks you will be undertaking in the lead up to the event. Obviously at this stage all Trekkers will have already completed their training and be fully conditioned and ready for the walk ahead. However no matter how much preparation you have done injuries still occur. What we frequently see at these events is with the excitement and adrenaline of the occasion Trekkers set off at too fast a pace making them vulnerable to blowing up or even injury. So make sure you have a strategy to ensure that you have a set pace and are able to stick to it. Researching the Route Being a coastal trek the course does include stretches of sand as well some climbs and descents. Knowing at what stage of the trek these harder sections will pop up will reduce the effect they have on your…
Thursday, 04 April 2019 21:59
Ankle Sprains - By Guy Agutter
Ankle sprains (aka “the rolled ankle”) present as the most common musculoskeletal injury in active populations and one we as physiotherapists see often. A sprain involves damage to the ligaments between the bones surrounding the ankle, and this is most commonly on the lateral side as these ligaments are not as strong as those on the inside of the ankle. Furthermore it is less common for us to roll our ankle ‘out’ compared to rolling our ankle ‘in’. Almost everyone has had these injuries at some point throughout their lives, and depending on the severity of the injury some may have healed completely or some people may have suffered ongoing ankle issues since. Pourkazemi et al. (2014) suggests that in the year following an ankle sprain you’re greater than two times more likely to re-injure the same ankle, with rates greater in those higher risk sports like basketball. Therefore it is crucial to follow a full rehabilitation program to help reduce these rates of recurrence and get yourself back to full function as soon as possible. Image courtesy of The American Board of Lower Extremity Surgery (2015) Injury Severity The degree of injury can generally be evaluated by your physiotherapist and can help us determine your return to sport or everyday function. These are: Grade 1 - Mild tear to the ligament. Grade 2 - Moderate tear of the ligament. Grade 3 - Severe tear or complete rupture of the ligament. Pain and swelling is generally localised to the injured ligament however initial swelling may make this less clear. The pain is worse with weight bearing and can generally be palpated by the physiotherapist. If the pain is higher up the ankle or lower down the foot you can suspect a differential or additional diagnosis. Pain is generally a poor…
More...
Tuesday, 05 February 2019 20:27
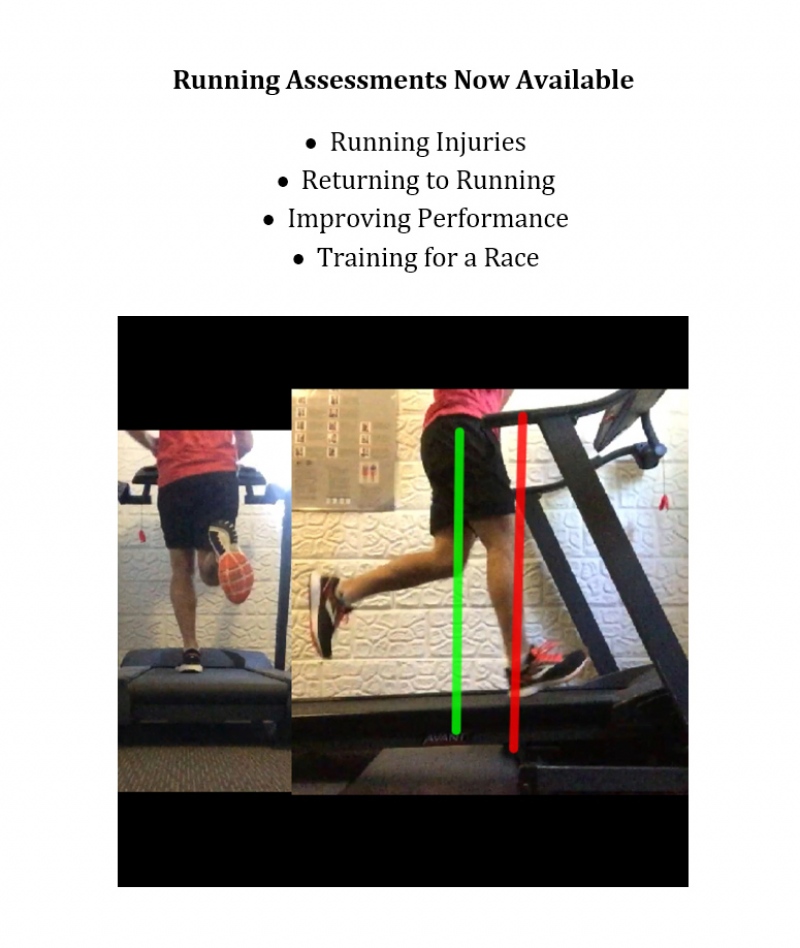
Is Running Safe for my Knees?
For a long time running has been associated with increased risks of degenerative hip and knee injuries, in particular Osteoarthritis (OA). This association has been so ingrained into public and professional perception that health practitioners have gone as far as advising people to avoid running in a bid to reduce the risks of OA changes. However these beliefs have been recently questioned when researchers compared a sedentary group of non runners with a group of recreational runners and found that the non runners suffered significantly more OA changes than the running group. It is important to note that these studies were carried out on healthy subjects with no pre existing knee injuries and also that when they looked into elite runners they found increased risks of OA changes. As health professionals these findings allow us to reassure patients that they can take advantage of the multiple health benefits of running and have less risk of OA than if they were sitting on the couch. Even if there are preexisting injuries to the knees we can get people back running with a suitable rehabilitation regime and a gradual return to running program. With our new running software at South Coast Physiotherapy we are now in the perfect position to offer assessments and programs to get people back running. Give the clinic a call and take advantage of all the benefits that getting back to running can offer.
Sunday, 02 September 2018 09:07
We are now a fully Registered NDIS provider
The National Disability Insurnace Scheme (NDIS) offers government support for people with disability, their families and carers. South Coast Physiotherpy is now fully registered with NDIS allowing us to provide physiotherapy services to those eligible.
Monday, 04 December 2017 22:00
Congratulations to Raquel
Big Congratulations to Raquel and her daughter Justine who completed the Arthurs Seat Challenge last weekend.