Physio Blogfrom the team at South Coast Physiotherapy

James Gasper
Warm up to reduce risk of Injury
Running & Arthritic Knees

Arthritic knee pain is very prevalent in the aging population and can lead to a reduction in activity at the very stage of life when we are trying to remain as active as possible. As physiotherapists a lot of our patient management is directed at keeping activities that will aggravate knee pain to a minimum and, at the same time, trying to keep the patient doing their hobbies and sports.
Old Wives Tales
Some sports and hobbies are more knee friendly than others but it is often not as straight forward as simply branding the ones that involve lots of knee impact as being the most dangerous. The old wives tale stating that too much running will lead to arthritis in the knees does not fit in with current evidence. Current evidence shows that individuals who run and have healthy knees are no more likely to suffer from arthritic changes than individuals who do not run.
Runners Vrs Non Runners
One study which supported this took knee x-rays of 50 year olds over an 18 year period. The subjects were split into a group that ran and a group that did not .The results showed no increased signs of osteoarthritic changes in the either group. Another study took an MRI of 7 runners before and after a marathon and they found that there were no signs of joint stress or deterioration after the race. Both these studies certainly point towards running not causing damage to the knee.
Further investigation into the effect of running on knees in animal studies showed evidence that running may have beneficial effects. A study in 1992 compared a group of dogs that ran to a control group that did not. They found that there was increased cartilage thickness in the groups that ran. Another study looked at mice over a 12 month period and found that a group who were kept active showed less signs of joint degeneration when compared to a group who had limited activity.
The evidence certainly sounds very clear cut but before you dig out your runners and head off to pound the pavements it is important to underline that the positive findings from these studies were mostly on individuals who have healthy knees.
Anecdotally, in the clinic, we certainly find that inactivity, be it spending long hours in the car or at a desk, is generally more detrimental to arthritic knees when compared to regular walking and sometimes even jogging. But I would strongly advise against heading out for a run as a way of attempting to reduce knee pain if you are not a regular runner and if you do not have a clear diagnosis of what is causing the pain.
Take Home Message
As with everything you read in books and on line, whether it is part of a gossip column or from a respected medical journal, the findings need to be related to your individual circumstances. As for arthritic knees we can recommend to people that they can continue running if they are a regular runner with no knee symptoms and that they will have no greater risk of degenerative changes compared to non runners. However if you have knee pain and are keen to start running or you are currently running with knee pain then I would recommend to have an assessment with a health care professional such as a physiotherapist to work on a safe running plan. Addressing factors such as running biomechanics, muscle strength, foot wear and the intensity and frequency of your running program all play a roll in implementing a safe running program. Ultimately, however, there will be levels of knee arthritis where running is not appropriate and in these situations it is important to look into more suitable exercises and activities.
Turmeric
Medical and Health care practitioners are advising more and more patients with inflammatory joint issues to take Turmeric as a natural form of pain relief. Although there has been a recent increase in the use of this herb it is not new and has been used for thousands of years in both Chinese and Indian medicine for a wide range of ailments including digestive complaints and chest pains.

Turmeric powder is the ground root of the turmeric plant and is what is responsible for the yellow colour in our curries. This yellow pigment is called Curcumin and is thought to be the primary pharmacological agent in Turmeric.
Anti-inflammatory properties
Curcumin has powerful anti inflammatory properties and its effects have been comparable to Ibuprofen but without the toxic side effects. However the amount of Curcumin in turmeric is low and therefore you would need to take large quantities for the desired effect. Luckily for us in the competitive and profit driven world of pharmaceuticals and natural medicines there are plenty of turmeric powders, tablets and capsules from numerous different companies.
There is no definite data or reliable studies at present comparing different brands and anecdotally the message from patients does not seem to point to one brand being better than another. However we do know that Curcumin is not well absorbed when taken orally and it is therefore recommended to take them with black pepper and iperine to aid absorption.
Joint Pain
The anti inflammatory properties of Turmeric make it a useful and safe way of managing inflammatory joint pain. A recent study found that a Turmeric supplement provided long term improvements in both pain and function in 1000 patients suffering from knee Osteoarthritis (OA).

Given the high prevalence of OA in our aging population and the associated problems it brings in regard to reduced activity and quality of life these positive findings will help future management of this condition.
Side Effects
Although Turmeric does not have the toxic side effects that are associated with other manufactured pain medication it does have side effects that people need to be aware of. It has been recommended to avoid using it in the lead up to surgery or when pregnant and high does can thin blood and therefore care needs to be taken when on any form of blood thinners. As with all medication, whether it is manufactured or natural, it is vital that your Doctor is aware of all the drugs you are taking and if in any doubt in regard to doses or brands then they should be consulted.
Conclusion
Turmeric has been around for a long, long time and used for various different ailments. Being a physiotherapist and working with musculoskeletal complaints I have focused on its anti inflammatory benefits and there is certainly scientific and anecdotal evidence that it has beneficial effects for inflammatory joint conditions. I therefore happily recommend it to patients with these complaints. The research is ongoing into what effects this drug has on the pathophysiology of certain diseases and I am confident in the months and years to come there will be more information regarding its benefits.
Nordic Walking – Skiing without the Snow…
I have recently been looking into Nordic Walking and its place as a treatment option for patients. This was after a surgeon had specifically recommended it to a patient for her rehabilitation post knee surgery. I have been aware of Nordic Walking for a number of years but have never involved it into rehab programs and therefore thought it would be a good area to look into and see if there is any evidence supporting its beneficial claims.
Nordic Walking is a total body version of walking, which has evolved from cross country skiers doing off season training. If you picture cross country skiing with no snow you have a pretty good picture of what it looks like.
I first came across Nordic Walking four years ago when a colleague was promoting it to her patients as an exercise that had all the benefits of walking with added upper body engagement. My colleague was a German physiotherapist who had seen the benefits of it back in Europe where it was a popular form of exercise.
Management and Treatment - Tennis Elbow
After being glued to the TV most evenings watching the Australian Open I thought a topical discussion for the beginning of 2016 would be the common elbow complaint known as tennis elbow. Now of course we all know that tennis elbow does not always involve tennis and in fact, in reality, tennis players only make up a small proportion of patients with these injuries.
Tennis elbow generally presents as pain on the outside of your elbow with gripping and lifting movements. The injury itself is to the tendons of the extensor muscles of the forearm and their attachments at the lateral epicondyle (which is the bony lump on the outside of your elbow). Generally the main muscle involved is the extensor carpi radialis brevis (ECRB).
Clinically we call this condition lateral epicondylagia and it is where the tendons (the structure that attaches the muscle to the bone) become worn down through excessive use, a little bit like a rope that has become frayed. This is called a tendinopathy. There can also be situations where the bony attachment also becomes involved which is called an ensthesopathy, but for this discussion we will focus on the tendon. The position of these structures can be seen in the diagram below.
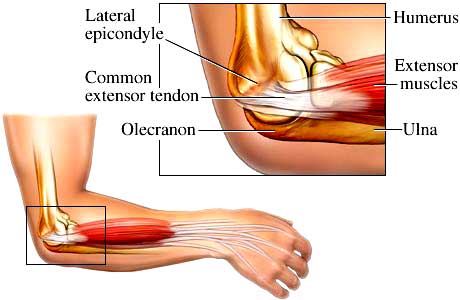
This condition is very common, with studies suggesting that 40% of people will experience some form of this injury through their lives. As well as being common these symptoms can take a long time to fully resolve with recent reports indicating it can be a number of years to be totally pain free.
It is most commonly experienced in the dominant arm and is a result of repetitive wrist extension. This can be from prolonged typing at a key board, a morning of lifting bricks in the garden or even a poor backhand technique in tennis!
Another important factor when looking at tennis elbow is the association it has with spinal and shoulder impairments. Evidence has shown that people with tennis elbow complaints are more likely to have neck pain than healthy counterparts. A link has also been found between weakness through the rotator cuff of the shoulder and tennis elbow.
However it is not all bad news. If the symptoms are diagnosed and managed early and there is minimal involvement of the cervical spine or shoulder then this condition does respond well to treatment and can have a good outcome. Therefore assessment is very important, as a clear diagnosis will give a good idea as to the prognosis of the injury. The table below gives a quick look at what presentations are likely to have the best outcomes.
|
Slow recovery |
Speedy recovery |
|
• Over 3 month history of pain
|
• Short history of symptoms - under 3 weeks
|
There are many different treatment modalities that we as physiotherapists have at our disposal to treat tennis elbow. I personally find joint mobilisations, dry needling and taping to be very beneficial and these treatments have evidence of being effective, particularly with patients who fit the 2nd column of the above table. However, one of the most beneficial intervention we can give as physiotherapists is education on the injury itself and correcting abnormal lifting or movement biomechanics which may have lead to the injury in the first place. This will often involve conditioning and mobility exercises for the spine or the shoulder, as well as the elbow and can result in changing a desk set up or a lifting technique.
To conclude, tennis elbow symptoms are very common and although they can often be unresponsive to treatments if you are able to get assessed by a physiotherapist in the early stages then you will have a greater chance of a better outcome. So the most important advice I can give is to get assessed by your physio or GP sooner rather than later.
Hamstring Injury Management & Prevention
We have all seen the classic hamstring injury where the sportsman or sportswoman puts in a sudden burst of speed towards a ball or away from an opposing player only to suddenly grab the back of their thigh with a grimace of pain etched across their face.
These injuries are very common in the sporting arena with studies showing hamstring tears being the most common soft tissue injury of all sports injuries. In the AFL they have been found to account for 16% of all injuries and 11% of all injuries in cricket.
There is a plethora of research into both the risk factors and the management protocols of hamstring injuries and yet they still fill up the treatment rooms of both professional and amateur sporting teams.
Risk Factors
As a physiotherapist an important part of our management is to be aware of the risk factors associated with these injuries and minimize them where possible.
Areas such as muscle strength, muscle imbalances, ankle mobility, biomechanics and endurance have been shown to have significant roles in hamstring injuries and they are areas that we can control with specific strengthening, conditioning and mobility programmes.
Other risk factors such as age, previous injury and the architecture of muscle tissue are out of our control but still need to be taken into account.
Assessment
When a hamstring injury first comes into the clinic there is pressure on the physio to get the patient back to their sport or back to their workplace as soon as possible. Unfortunately all soft tissue injuries need to be allowed time for the body to heal them and there is generally very little that can be done to speed this process up. Depending on the severity of the tear these time frames can vary, with a low grade tear taking only a couple of weeks to a higher grade tear taking over 3 months.
Depending on where in the muscle complex the tear has occurred will also be a factor in how long it takes for the patient to return to their activity. For example a tear near the top of the muscle where it joins into the pelvis and where the fibers are more tendinous will generally take longer to heal than a tear in center of the muscle belly.
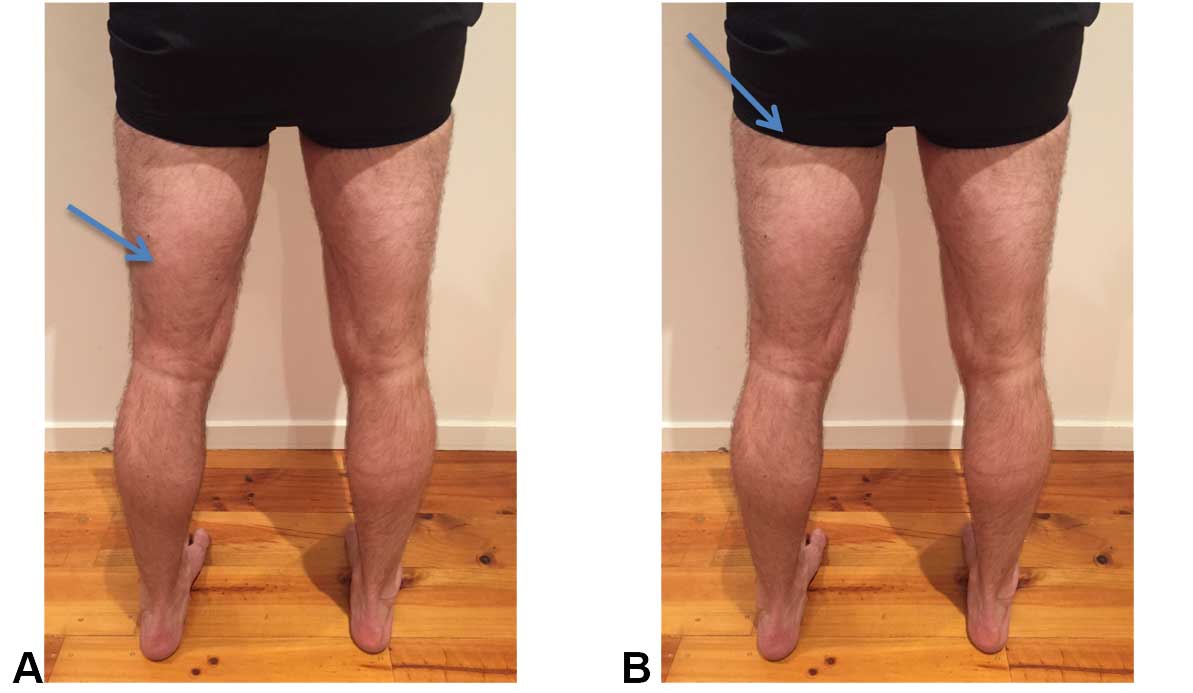
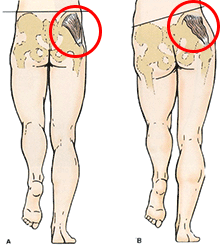
A tear in the muscle belly (as shown by the arrow in pic A) will have a greater healing capacity than a tear which is nearer the insertion of the muscle (arrow in pic B). One of the reasons for this is the greater blood supply in the muscle belly compared to at the insertion.
A thorough assessment with your physiotherapist should be able to differentiate between these different grades of hamstring injuries and the different regions where the injury has occurred. From which an initial treatment plan and an expected time frame for return to sport (or work) can be set.
Treatment and Conditioning
The general acronym for the management of soft tissues injuries is PRICE standing for Protection, Rest, Ice, Compression and Elevation. This blue print for the initial management of these injuries has stood the test of time well and is a good way of managing early hamstring tears. However the current research looking specifically at hamstring injuries suggests that they respond positively with early movement and mobilization as this promotes early muscle regeneration. Therefore following the acute stage of a hamstring injury (generally after the first 24hrs to 3 days) the acronym commonly used for ongoing management is POLICE, which stands for Protection, Optimal Loading, Ice, Compression and Elevation.
As the hamstring improves and can tolerate more load a graded loading and mobility program is essential for a return to sport or the workplace. A study comparing a purely stretching and strengthening program to an agility and trunk stabilization program found the latter to be far superior in preventing recurrence of hamstring tears. This program needs to be tailored to each individual and to the movements and loads that are associated with the activity they are wanting to get back too.
Summary
To summarize, hamstring tears are one of the most, if not the most, common sporting injury. There are a long list of risk factors which will make you more vulnerable to injury. Some of these can be managed through specific exercises, strengthening and mobility programmes. Others we cannot change but we also shouldn’t ignore. The correct diagnosis of the type and severity of injury is then vital to ensure you can undertake the most suitable management plan enabling a return to activity and minimizing the risk of re-injury.
I hope this is of some help to people who have had or are having hamstring issues. It is certainly beneficial to get professional help through this process from physiotherapists or sports doctors in order to get back to sport as quickly as possible while minimizing the risk of future injury.
To stretch or not to stretch?
One of the most frequent questions I get asked is in regard to the correct stretching protocol when warming up for sports or at the gym. What type is best? When should they be done and for what duration?

Types of Stretches
As with many questions regarding the human body, the answer is dependent upon numerous variables and giving a generic stretch protocol is difficult. As physiotherapists we use many different types of stretches including static, dynamic, ballistic, proprioceptive neuromuscular (PNF)and many more. They are generally used to help the body achieve the necessary movement and mobility needed for the task it is trying to perform. Not only do they often form an integral part of a patient’s treatment, but they are also vital in reducing future injury risk.
As a result of the flourishing fitness, health and wellbeing industries there is ongoing research into all different types of stretches which is giving us an ever increasing knowledge base into this area. As a result advice on the correct stretching protocol is continually being updated.
Variables
When deciding what to prescribe for a patient it is important to know what type of activity they are undertaking. For example you would not do the same stretches before you take your first golf swing as you would if you were trying to increase your knee mobility after surgery. On top of this the age of the person doing the stretch needs to be taking into account, as the properties of the structures we are stretching will change with age and therefore will respond differently.
These are only a few of the long list of variables that would need to be addressed when giving advice on stretches and it gives an indication how trying to have a generic ‘one size fits all’ stretch is probably inappropriate.
Static Stretch

One of the most common stretches that are used through gyms and in sport is the static stretch. This involves holding a muscle in an elongated position for a sustained period. Recently these stretches have had some bad publicity with research showing that when undertaken before activity they can lead to reduced muscle strength and can hinder physical performance.
However the negative effects of these stretches are generally only observed when the stretches have been done in isolationand not part of a general warm up routine or when they have been held for over 60 seconds. When shorter duration stretches are undertaken as part of a pre-exercise routine evidence shows no compromise to muscle performance. There is also evidence that shows when, even in isolation, static stretches that are held for under 60 secondshave no negative effects, with one study finding that they actually increased leg extension power. However I think warm up routines are vital in preparing yourself for all levels of activity, whether it is for a morning of gardening or for a grand final and therefore I rarely recommend static stretches in isolation
Conclusion
I do not think there is enough evidence to advise people to stop doing static stretches but when they are used they should be held for less than 60 seconds and should be incorporated in a warm up routine rather than in isolation. Having said that I also do not think they are vital and if you have been someone who has never stretched before activity there is no overwhelming evidence that suggests you should start although I would recommend to do some form of warm up.
This advice is, however, dependent on injury. If you have an injury, either an old one or a new one, certain warm ups or stretches may be inappropriate. Therefore if you are in a position where you are looking for stretches to bring into your warm up routine because of an injury, or if you are returning to sport after an injury, then I would strongly advise to have a full assessment from a physiotherapist and get a diagnosis and a specific set of exercises or stretches.
Skiing injury Prevention
With both Australia and New Zealand having good snow seasons this year and following a recent run of patients suffering snow related injuries I have decided to write this blog on injury prevention when on the slopes.
Risk of Injury
Although skiing and snow boarding are generally associated, as high injury risk activities recent research looking at the prevalence of these injuries has shown a recent decline. The numbers have reduced from 5 – 8 injuries per 1000 skiers to 2 – 3 per 1000.

Research has also shown that the most common injuries in skiing are to the knees which accounts for ⅓ of all injuries and that in snowboarder’s injuries to the wrists are the most common. A study in Japan showed that snowboarders had twice the injury rate of skiers and interestingly a study looking at a terrain park in Canada showed that snowboarders who were listening to music were less likely to have an any injury but more likely to have an injury which resulted in them being taken to the emergency department!
When looking at preventing injuries there are obviously areas that we have no control over, which can increase the chances of injury. These can include poor visibility, the quality of the snow and crowded pistes. However there are also many areas that we can control such as wearing protective garments including wrist protectors and helmets.
Conditioning
One area that has been proven to reduce injuries in skiing is through skiing specific physical conditioning. With snow based disciplines, as with the majority of sports, it is important to be balanced and maintain good alignment and weight distribution through your trunk and lower limbs. However, unlike a lot of other sports, with skiing you are trying to maintain a relatively static position while travelling fast down a hill. This, therefore, is going to require different muscle activity and joint positioning compared to an activity such as running, meaning a specific conditioning program is necessary.
Alignment
When looking at skiing you need to assess your alignment to avoid excessive loading through your knees and hips. A lot of pain experienced through the front of the knee with skiing is a result of over loading through the patella femoral joint (where the knee cap sits). When you go into your skiing position your knees should be in line with your 2nd to 3rd toes and not dropping in towards the inside of your big toes. (as shown in the figure below)

Knee dropping inside the big toe: incorrect Knee in line with the 2nd to 3rd toes: correct
Once you have addressed this imbalance it is then important that you are achieving the correct hip and knee movement. As you go into the skiing position your weight needs to be more into the front of your feet rather than at the back as this will distribute your weight in a more uniform pattern through your skis giving you greater control. This is slightly different to the sit stand motion we use on a daily basis where our weight is distributed more through our heels and therefore it can take a little bit of training to get right.
Strength
In order to maintain this alignment it is vital to have good strength through the gluteal and quadriceps muscle groups. Due to the down hill nature of skiing the quadriceps need to be worked eccentrically. This means they are worked from a straight knee position to a bent knee position and the quadriceps muscles are lengthening. Two of the best exercises to achieve this are deep squats and vertical split squats (as shown below).

Vertical Split squats
Proprioception & Endurance
Proprioception is the body’s awareness of where it is in space and is therefore a very important factor in reducing injury risk, especially when skiing in poor visibility. Simple ways to address this are through balance exercises such as single leg standing with eyes closed.
Similar to other sporting injuries, skiers and snow borders are more vulnerable as they get more fatigued and this can be addressed through generic cardiovascular exercises such as cycling and running.
It is important to mention that these guidelines are for uninjured skiers. If you have an ongoing complaint or old injury then a more specific personal program would be necessary.
Happy Skiing……
Lateral Hip Pain
Following on from my previous blog about golf injuries, I thought I would look at another common complaint. Lateral hip pain is certainly one of the most common problems we see walk through the door and it is also one of the most frustrating to treat and manage.
What is Lateral Hip Pain?
Firstly, there are many different structures that could be causing pain through your hip such as osteoarthritic changes, your Sacral Iliac Joint (SIJ) or your lower back so it is important that you have a full assessment in order get the right diagnosis from the start.
The condition I am going to discuss is trochanteric pain syndrome and the role the gluteal tendons play in it. This syndrome can cause pain on the outside of the hip, which can spread down to the knee and run into the buttock.
Generally these symptoms are aggravated with prolonged walking, going up and down stairs and lying on the involved side. Initially these symptoms where often thought to be associated with inflammation to the bursa on the side of the hip. This was known as trochanteric bursitis. However with improvements in investigations such as MRI and Ultrasound clinicians now believe that the tendons of the gluteus medius and the gluteus minimus muscles are more involved. We believe that the pain that is experienced is a result of these tendons being over loaded and losing their structural integrity resulting in them breaking down. This condition is known as a tendinopathy.
How does this happen?
This overloading of the tendons on the outside of your hip is often the result of poor control and balance through the pelvic and lower back regions. On assessment there is often a weakness through the muscle groups that are associated with stabilizing the hip joint. A simple way of assessing this is to look at how well the patient is able to balance on 1 leg. The picture below shows how an unstable pelvis will tilt on a single leg stand and put pressure on the gluteus medius muscle.
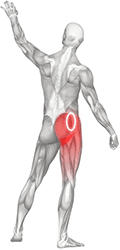
Gluteus Medius
When looking into the history of our patients with this injury there is generally an episode of increased loading or an increase in activity, such as a day in the garden or starting a new exercise group. This spike in activity can aggravate the tendons of the gluteus medius and minimus muscles if there is not suitable stability through the pelvis. Once these tendons have been aggravated they are then easily re-aggravated during daily activities such as going up and down stairs or from sleeping on the affected side.
Recommended Therapies : Dry Needling
A major part of physiotherapy intervention for trochanteric pain is based on correcting this imbalance, which can be done through specific strengthening and conditioning programs. However, before any of these exercises can be implemented it is important for the pain levels to be well controlled and this is where dry needling comes in. There are many treatments that are used to control pain levels and sometimes it is necessary for medical intervention, but I find Dry Needling is an effective option.
What is Dry Needling?
Dry needling is where acupuncture needles are used in specific regions of different muscle groups to inhibit and suppress how the body processes pain. Unfortunately the longer the pain has been present the longer it takes to control and therefore time frames can vary. Once the pain levels are controlled then we can introduce specific loading exercises for the tendon and ultimately a full strengthening program to restore pelvic stability.
As I mentioned at the beginning, this can be a very frustrating condition to treat and to get on top of. In chronic conditions where pain has been present for a number of months it is often necessary for onwards referrals to medical practitioners to get to a position where a conditioning program can be tolerated. Therefore it is important to get an early assessment and diagnosis.
Physiotherapy and Golf
My name is James and I am one of the lead physiotherapists at South Coast Physiotherapy. I would like to welcome you to my first ever blog for which I have decided to write a little about a common complaint which I am regularly treating at the clinic. Living on the Mornington Peninsula we are fortunate to have a plethora of high quality golf courses. Golf is a great past time which offers the perfect low impact exercise which, as physiotherapists, we encourage our patients to partake in.
There are, however, injuries associated with playing golf and none more common than low back pain which has been found to make up 25% of all golf related injuries and is certainly an injury we see a lot coming through the doors at the clinic. Interestingly low back pain has not only been shown to be the most prevalent golfers injury but also has been shown to have a significant effect on the efficiency of a players swing with research showing back pain reduces downswing velocity by up to 50%.
One of the reasons for the prevalence of these low back injuries is the biomechanics associated with the golf swing. The golf swing involves an asymmetrical rotational velocity with the slow back swing going away from the body and then a fast and powerful downswing in the opposite direction. This creates an imbalance through the lower back (lumbar spine) with one side of the spine being put under more stress than the other.
Added to this imbalance is the repetitive nature of the golf swing. Be it with taking numerous practice swings before each shot during a round of golf or with going through a bucket of balls on the driving range, an average golfer is going through a high number of golf swings on each outing. This high repetition, along with the natural biomechanical imbalance of a golf swing, creates the perfect storm in regard to either disc or facet joint injuries to the lumbar spine. It is therefore vital to reduce this risk by ensuring that your lumbar spine has both the necessary stability and mobility to tolerate these loads.
Studies looking at these lower back injuries have shown that by assessing the golfer’s spinal mobility and the stability of the pelvis and trunk you can have an idea of how vulnerable they are for these injuries. Two of the major areas we look at as clinicians is the rotation through the mid back area (the thoracic spine) and muscle power through the oblique and transverse abdominal muscle groups. Golfers who maintain good trunk rotation through their thoracic spine and equal muscle power through their abdominals are less likely to have lower back issues.
Added to this are the unavoidable daily activities such as work, driving and family commitments that can add to these risk factors. Either prolonged sitting at work or in the car will lead to increased spinal stiffness and the tight time scales of a busy family life can mean that there is less opportunity to do warm exercises or mobility and conditioning work.
Therefore I have found that individualised programmes based on a players specific deficits in either spinal movement or core strength which take into account these added risk factors has been the best way of managing low back pain and minimising the risks of future injury.
Thank you for reading my first ever blog and I hope it has been an interesting and informative read. If you have any queries regarding golf related back injuries then please get in touch and I would be happy to help.